The abbreviation MRI stands for magnetic resonance imaging. It is a type of medical imaging technology that produces highly detailed images of the anatomy and physiological processes in the body — especially soft tissues like the brain, muscles, and organs. MRI scanners use strong magnetic fields and radio waves to form images of the body. MRI is widely used for the diagnosis, staging and follow-up of disease.
Our Journey to the Region’s First MRI
Now taking referrals!
Healthcare providers can access the requisition from our Diagnostic Imaging page.
Muskoka Algonquin Healthcare (MAHC) is proud to deliver high quality, patient-centred care through the arrival of the Muskoka region’s first donor funded Magnetic Resonance Imaging (MRI) machine at the Huntsville District Memorial Hospital (HDMH) Site.
Thanks to the generosity of our community through funds raised by the Huntsville Hospital Foundation’s Focus on Imaging campaign, access to MRI scans will be closer to home than ever before with operational funding for MRI provided by the Ministry of Health.
The arrival of our region’s first MRI means enhanced diagnostics and access to more advanced healthcare for the residents of Muskoka and Almaguin. Getting an MRI locally means you won’t have to travel as far – in fact we anticipate this will save our patients over 7,000 hours behind the wheel and 700,000 kilometers of travel to hospitals outside of our region for an MRI.
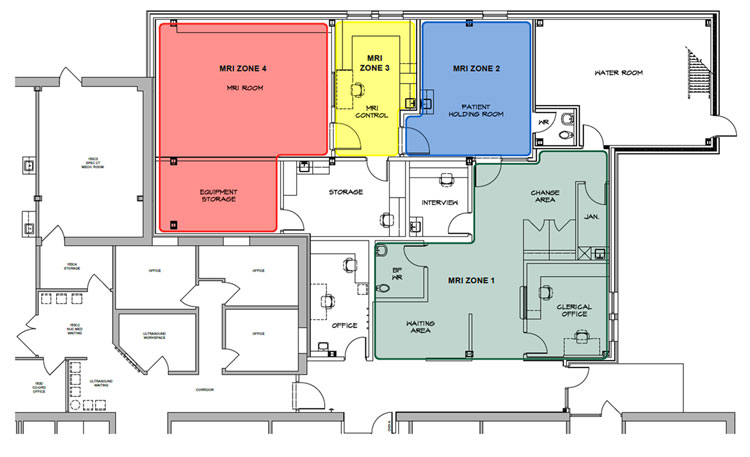
The MRI service opened on July 7, 2025 in a 3,700-square foot addition behind the Emergency Department. Healthcare provider will be able to provide a referral for the following services:
- Breast MRI
- Musculoskeletal MRI
- Neuro (brain and spine) MRI
- Pelvic / Abdominal MRI
- Prostate MRI
At its maturity, Muskoka and area’s MRI service will complete 5,000 MRI scans locally every year.
From the Ground Up
In December 2022, the provincial government announced that MAHC was one of 27 Ontario hospitals to receive operational funding for a new MRI machine at the HDMH Site.
In July 2024, joined by donors and dignitaries, we marked the official start of construction with a groundbreaking ceremony that followed months of behind-the-scenes planning. This involved the architectural design of the space, contractor tendering for the construction of the MRI Suite, special designation to operate magnetic resonance, and selection of the Siemens vendor to build MAHC’s first MRI machine.
Nine months of construction, including an essential planned power outage to connect the MRI Suite to the hospital’s power system, is turning a shell of space into a fully operational, state-of-the-art patient care area that will enhance diagnostic capabilities and patient care for years to come.
On July 7, 2025, the MRI Suite opened and accepted its first patient.
Construction Progress & the MRI Machine's Arrival
Nine months of construction, including an essential planned power outage to connect the MRI Suite to the hospital’s power system, is turning a shell of space into a fully operational, state-of-the-art patient care area that will enhance diagnostic capabilities and patient care for years to come. Learn more about our progress and check out our photo gallery from January to May 2025.
In May 2025, our donor-funded MRI machine travelled from Erlangen, Germany to Muskoka where it was lowered by crane and installed in the MRI Room within the new MRI addition in Huntsville. As finishings such as flooring, painting, IT network cabling, millwork, furniture and fixtures are completed, the MRI machine is going through testing and commissioning with the machine fully functional in July.
Fundraising Journey
Announcing Muskoka’s first MRI in Huntsville was big news! Raising the funds required to purchase the new MRI machine was an even bigger challenge — one that the community met with incredible generosity, determination, and a shared commitment to improving local healthcare. The MRI is the result of a concerted effort by the Huntsville Hospital Foundation for community fundraising to the tune of $7.5 million as part of the Focus on Imaging campaign. The campaign generated 2,460 donations from residents, businesses and community groups from South River to Orillia and Haliburton to Parry Sound in only three years, a relatively short period of time for a campaign like this.
Meet the Team
We are excited to introduce the exceptional team behind Muskoka’s first MRI Suite in Huntsville. They are a group of highly skilled radiologists, technologists, and support staff dedicated to delivering top-tier diagnostic imaging with compassion and precision. Carefully selected for their expertise and commitment to patient care, this new team is ready to bring advanced imaging services closer to home, ensuring faster diagnoses and improved health outcomes for the entire community.

Dr. Maneesh Gupta, MD. FRCPC
Radiologist, Magnetic Resonance Medical Director
Dr. Gupta completed his medical degree and diagnostic radiology residency at the University of Toronto, as well as a fellowship in Magnetic Resonance Predominant Body Imaging and Musculoskeletal Imaging at Northwestern University. He has worked as a radiologist at Scarborough Health Network (SHN), Lakeridge Health (LH), and Muskoka Algonquin Healthcare since 2014. He has been the MRI Section Head at SHN and LH since 2019. He is trained as a software engineer and has a special interest in health-related information technology and systems design.

Dr. Jason Blaichman, MDCM. FRCPC
Radiologist, Chief & Director of Diagnostic Imaging
Dr. Blaichman joined MAHC in 2019 and has been serving as Chief and Director of Diagnostic Imaging since 2022. Dr. Blaichman earned his Medical Degree from McGill University and completed his Diagnostic Radiology Residency at the University of Toronto. He subsequently undertook a Fellowship in Musculoskeletal Imaging and Intervention at the University of Wisconsin-Madison. Dr. Blaichman’s subspecialty interests include musculoskeletal MRI and ultrasound and image-guided pain management, including spine intervention. He holds an academic appointment as an Adjunct Lecturer with the University of Toronto.

Muhammad Tajammul, MRT
MRI Technologist
With a degree in Medical Imaging Technology and more than 20 years of medical imaging experience including specialized training in MRI, Muhammad began his professional career as an MRI Technologist at The Aga Khan University Hospital, a leading institution recognized for its advanced imaging equipment and international accreditation. During his decade there, he gained valuable experience in a wide range of MRI procedures, developed strong technical skills, and enhanced his patient care abilities while maintaining high standards of imaging quality and safety.
In 2013, Muhammad relocated to the Kingdom of Saudi Arabia where he continued his career as an MRI Technologist at the Ministry of National Guard Health Affairs, facilitating both routine and complex MRI procedures on multiple state-of-the-art MRI systems in a dynamic hospital environment. He trained junior staff, helped optimize protocols and safety practices in a high-volume environment, ensured compliance with MRI safety guidelines, and participated in department quality improvement initiatives. This experience further strengthened his clinical expertise and adaptability in an international healthcare setting.
Originally from Pakistan, he immigrated to Canada in 2023 to build a better future for his family and new professional and personal opportunities. He initially settled in British Columbia where he was inspired by the country’s natural beauty, multicultural environment, and supportive community. Muhammad and his wife and three children recently moved to Muskoka and have settled in well. The family is delighted with the region’s family-friendly environment and is excited about their future here in Muskoka.

Manon Leveille, MRT
MRI Technologist
Manon has been a Medical Radiation Technologist in Northern Ontario for 15 years with 11 years’ experience working in MRI. Manon acquired her MRI experience from the Sault and Area Hospital and the North Bay Regional Health Centre. Manon is excited to join Muskoka’s MRI team and be part of a brand-new MRI department. In her spare time, Manon enjoys spending time with family and doing outdoor activities.

James Norrie, MRT
MRI Technologist
James recently moved to the area from Timmins, where he worked as an MRI Technologist at the
Timmins and District Hospital. James graduated from the MRI program at Cambrian College in 2023 and
completed a four-year Bachelor of Science Degree with specialization in Biomedical Biology at Laurentian
University prior. When he’s not working, he enjoys spending time outdoors — often cross-country skiing,
hiking, and mountain biking.

Carla Salameh
MRI Registration & Scheduling Clerk
Carla first joined the MAHC team in 2022 and returned in July 2024, working as a Diagnostic Imaging Clerk. She holds a degree in Biomedical Sciences from Trent University. Having scored 97% on her Medical College Admission Test, Carla has set her sights on starting medical school in September 2026 with a goal of becoming a pediatric surgeon. Carla speaks five languages and is a certified elementary grade level tutor in math, biology, and French. As part of the Central Patient Registration & Scheduling team, she is excited by her upcoming assignment as a patient registration and scheduling clerk in the new MRI Suite.

Michelle Beaver
MRI Registration & Scheduling Clerk
Michelle joined the MAHC team in November 2024 as a Diagnostic Imaging Clerk. Prior to her current role, she served as the Coordinator of a community-based mental health program for over 20 years where she built a strong foundation in patient support, advocacy and care. She holds an Office Administration Diploma and a Medical Terminology Certificate.
Michelle is known not only for her wealth of knowledge and experience, but also for her deep empathy and kindness – qualities that shine in every patient interaction. As a cancer survivor and someone who has personally navigated the healthcare system, she brings an authentic, compassionate perspective that helps reassure patients they are in capable and caring hands.
In her spare time, Michelle enjoys spending as much time as possible outdoors with her family, and is on a mission to discover which flowers will thrive in her garden!
Frequently Asked Questions
What is MRI and how does it work?
The MRI is located at Huntsville District Memorial Hospital where the region’s District Stroke Centre is also located. It is installed within a 3,700 square foot addition behind the Diagnostic Imaging and Emergency Departments.
The new MRI is expected to open for patient services in July 2025, operating five days a week.
When the hospital is redeveloped what will happen to the MRI?
Bringing an MRI to Muskoka has been a long-time goal, and we're thrilled that patients will soon have access to this service. The new MRI will continue to make a big difference for thousands of people each year, even as we work toward approvals for our new hospitals. An MRI is certainly part of the plans for the future hospital, and when the time comes, decisions about the machine will consider its age, condition, and any new advances in technology to ensure we’re providing the very best care possible.
Yes, MRI is extremely safe. Unlike X-rays and CT scans, there is no radiation involved in an MRI. Technologists carefully screen each patient prior to the scan to ensure they are safe to enter the scan. This involves screening for metal, such as devices with metal in them – like a pacemaker, metal plates, rods or screws from surgery, or even piercings. MRI Technologists are highly trained professionals who have extensive knowledge and training to operate the scanner safely under all conditions. During some procedures, a common side effect during the scan can be a warming sensation of the body area being scanned. There are techniques technologists use to adjust parameters to minimize the effects of warming to ensure you are kept safe and comfortable.
MRI is an effective test for detecting and staging cancer in many parts of the body. This includes brain, spine, breast, lung, bladder, pancreas, liver, esophagus, and prostate, as well as multiple myeloma and non-Hodgkin’s lymphoma. However, there are limitations, and this is why your doctor may order other tests to make a cancer diagnosis. No matter what kind of cancer your doctor thinks you have, you may have multiple tests done to confirm the diagnosis. The process could include blood and urine testing, other imaging tests, endoscopy, biopsy, and genetic testing. MRIs are often an important part of this process.
Is it safe to have an MRI if I am pregnant?
Physicians use a benefit versus risk model when ordering MRI scans. What are the benefits and what are the risks? Lots of research has been carried out into whether the magnetic fields and radio waves used during MRI scans could pose a risk to you or your baby. Typically, MRI scans are safe during the second and third trimesters. MRI scans are generally not performed during the first trimester unless the benefits outweigh the risks. This is the ensure that anyone who is pregnant, including their fetus, is always kept safe. Our multidisciplinary team of medical experts will discuss options with you so that you can make an informed decision prior to undergoing an MRI procedure.
Can I have an MRI if I have a pacemaker? What if I have metal implants or prosthetics?
Yes, modern-day tattoos are predominantly safe for MRI scanners. Our staff are trained to determine on a case-by-case basis whether a tattoo requires further investigation before imaging. Permanent makeup tattoos, such as permanent eyebrows and lip line tattoos, are generally safe but may require the technologist to take additional cautionary steps when scanning. The age of a tattoo is also taken into consideration. Tattoos from the 1950s to 1980s, where inks may have included metallic components, are further assessed based on colour, shape, and the area of the body being scanned relative to the location of the tattoo. Some colours are more dangerous than others — for example red ink is more magnetic than other colours. Red inks may contain iron which conducts electricity, possibly resulting in burns during an MRI. Tattoos in the shape of a loop or circle can act like an antenna to the radiofrequencies when having an MRI and have the potential to conduct heat and also result in a burn. Having a tattoo does not prevent you from having an MRI.
How long will I be in the MRI scanner?
Imagine an unsliced loaf of bread. When it is sliced in half, you can see inside the loaf, but you don’t see as much as you would if there were many slices and each slice was 1-5 mm thick. In this case, you can look at the entire loaf in much more detail one slice at a time. In MRI, we use what is referred to as a sequence to take an image of the body. In a single sequence, there may be up to 40 slices, each slice taking from less than one second up to 20 seconds. The total time spent in the scanner depends on the body part that is being scanned. The larger the loaf of bread, the more slices we will have. Similarly, the larger the body area being scanned, the more slices that are required, thus requiring more time. During the MRI, we also look at the human body in different planes, for example, top-to-bottom, left-to-right, and front-to-back, compared to a CT scan which only scans from top-to-bottom. Imagine how many tiny cubes of bread if we sliced the loaf of bread this way. To save time, certain sequences form a 3-dimensional image which saves time. Multiple sequences are required for each MRI exam as each sequence shows the anatomy differently. The average sequence lasts three to five minutes. The shortest scans are usually about 20 minutes. An MRI of the abdomen may take up to 60 minutes. That might seem like a long time but this allows the doctors to visualize your anatomy in detail, looking at thousands of little cubes, helping them write a detailed MRI report for your physician.
Sign up to our Muskoka Health Matters Newsletter
Stay up to date on the hospital’s programs and services, events, and other announcements by subscribing to our eNewsletters.

























